Venture into the intricate landscape of your mouth, and you’ll discover it’s far more than just teeth and a tongue. It’s a complex environment, lined with different types of soft tissues, each with its own unique characteristics and purpose. Among these, there exists a subtle yet profoundly important boundary line, a demarcation that plays a critical role in the health and function of your oral cavity. This line is known as the mucogingival junction, often abbreviated as MGJ. While it might not be something you consciously notice every day, its presence is fundamental to how your gums and the inner lining of your mouth work together.
Unveiling the Boundary Line: What is the Mucogingival Junction?
The mucogingival junction is an anatomical feature found in the oral cavity. Think of it as a visible line or a transition zone where the specialized gum tissue firmly attached to your teeth and jawbone meets the more delicate, movable lining of your cheeks and lips. This junction isn’t just a random line; it represents a significant change in tissue type, structure, and function. It typically appears as a scalloped line that follows the curves of your teeth and gums, more apparent in some areas of the mouth than others. Understanding this junction is key to appreciating the sophisticated design of our oral anatomy.
You can find this junction on both the upper (maxillary) and lower (mandibular) jaws, on the facial (cheek/lip) side and sometimes on the lingual (tongue) side of the lower jaw. Its exact position can vary slightly from person to person and even from tooth to tooth within the same individual. The clarity of the MGJ can also be influenced by factors like pigmentation and the overall health of the oral tissues.
The Tissues at Play: A Tale of Two Mucosas
To truly grasp the significance of the mucogingival junction, we need to look at the two distinct types of tissues it separates: the attached gingiva and the alveolar mucosa.
The Resilient Attached Gingiva
Located on the tooth-side of the MGJ is the attached gingiva. This tissue is part of the broader gingiva, commonly known as your gums. The attached gingiva is specifically the portion that is firmly bound down to the underlying periosteum (the membrane covering the bone) of the alveolar bone – the bone that supports your teeth. Let’s explore its key characteristics:
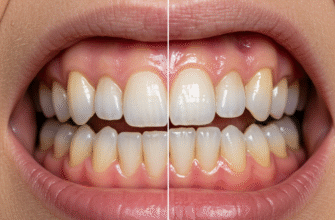
- Appearance: It is typically pale pink in color, though this can vary with natural pigmentation. A healthy attached gingiva often has a stippled texture, somewhat resembling the surface of an orange peel. This stippling is due to the way the connective tissue fibers attach the epithelium to the bone.
- Consistency: It is firm and resilient to the touch. It doesn’t move when you pull your lip or cheek.
- Composition: The surface layer is made of keratinized stratified squamous epithelium. Keratin is a tough, fibrous protein (the same protein found in your skin, hair, and nails) that makes this tissue resistant to the friction and pressures of chewing and brushing.
- Function: Its primary role is protection. It safeguards the underlying bone and the roots of the teeth. It also helps to withstand the mechanical stresses of mastication (chewing) and oral hygiene practices. The attached gingiva provides a stable cuff around the necks of the teeth, contributing to the overall stability of the periodontal structures.
The width of the attached gingiva can vary throughout the mouth. It is generally widest in the incisor regions and narrower in the posterior (molar) regions, especially around premolars.
The Flexible Alveolar Mucosa
On the other side of the mucogingival junction, extending away from the teeth towards the inner cheeks, lips, and floor of the mouth, lies the alveolar mucosa. This tissue is distinctly different from the attached gingiva.
- Appearance: It is typically a darker red, shinier, and smoother in appearance compared to the pale pink, stippled attached gingiva. The redder color is due to the presence of more numerous blood vessels closer to the surface and a thinner epithelial layer.
- Consistency: It is thin, soft, and highly movable. You can easily see it stretch and move when you move your lips, cheeks, or tongue.
- Composition: The surface layer is made of non-keratinized stratified squamous epithelium. The absence of a significant keratin layer makes it more delicate and less resistant to abrasion than the attached gingiva. Its underlying connective tissue is also looser, allowing for greater flexibility.
- Function: Its main purpose is to allow for the free movement of the lips and cheeks during speech, eating, and facial expressions. If this tissue were as firm as the attached gingiva, these movements would be severely restricted and could potentially pull the gums away from the teeth.
The mucogingival junction is readily identifiable by a distinct color shift, moving from the paler pink of the attached gingiva to the deeper red of the alveolar mucosa. This visual cue is complemented by a change in texture and mobility. The attached gingiva is firm and stippled, while the alveolar mucosa is smooth and easily movable. These differences highlight their distinct functional roles within the oral cavity, one providing robust protection and the other offering essential flexibility.
Why This Line Matters So Much: The Functional Significance
The mucogingival junction isn’t just a passive landmark; it’s an active player in maintaining oral harmony. Its existence and proper location are crucial for several reasons:
1. Barrier Function: It acts as a clear boundary, separating the tough, masticatory mucosa (attached gingiva) designed to withstand wear and tear from the delicate lining mucosa (alveolar mucosa) designed for mobility. This separation ensures that each tissue can perform its specialized role effectively without interference from the other.
2. Gingival Stability: The firm attachment of the gingiva to the bone, demarcated by the MGJ, is vital for keeping the gums stable around the teeth. This stability helps prevent the gums from being easily stripped away from the teeth during chewing or vigorous brushing. If the alveolar mucosa extended all the way to the teeth, the gums would be far too mobile and prone to injury and recession.
3. Facilitating Movement: Conversely, the alveolar mucosa, beginning at the MGJ, allows for the necessary movement of the lips, cheeks, and tongue. Imagine trying to smile or speak if the lining of your cheeks was as tightly bound as your gums. The MGJ ensures there’s a transition to a tissue type that can accommodate these dynamic actions without exerting undue pulling forces on the gingival margin (the edge of the gum around the tooth).
4. An Anatomical Guide: For dental professionals, the MGJ is an important anatomical reference point. Its location helps in assessing the width of the attached gingiva. An adequate band of attached gingiva is often considered important for maintaining periodontal health, although the exact amount needed can be a subject of debate and varies per individual. Changes in the position of the MGJ relative to the tooth can indicate processes like gingival recession.
Spotting the Junction: How to Observe the MGJ
While it takes a trained eye to fully appreciate all its nuances, you might be able to observe the mucogingival junction in your own mouth, or at least understand what a dental professional looks for. The primary indicators are:
- Color Change: This is often the most obvious sign. Look for the line where the lighter pink gum tissue meets the deeper red, more vascular-looking tissue of your inner cheek or lip lining.
- Texture Difference: The attached gingiva often has that stippled, slightly rougher texture, while the alveolar mucosa is smooth and shiny.
- Mobility Test: A dental professional might gently retract the lip or cheek. The alveolar mucosa will move freely, while the attached gingiva will remain fixed. The line where this difference in movement occurs is the MGJ. This is often best visualized by applying air from a dental syringe, which can dry the tissues and make the contrast more apparent, or by using a periodontal probe to gently push the alveolar mucosa and see where it begins to move independently of the gingiva.
Observing the MGJ is a standard part of a comprehensive oral examination. Its appearance and location can provide valuable information about the patient’s periodontal architecture.
Considerations and Variations
The mucogingival junction isn’t static throughout life, nor is it identical in every person or every part of the mouth. It forms as teeth erupt and the different oral tissues differentiate. The width of the attached gingiva, defined by the MGJ and the base of the gingival sulcus (the small pocket between the tooth and the free gingiva), can change over time. For instance, if gingival recession occurs (where the gum line pulls away from the crown of the tooth), the band of attached gingiva may narrow, bringing the MGJ closer to the gingival margin.
In some cases, particularly where teeth are very prominent or there’s a strong pull from muscle attachments (frena), the zone of attached gingiva might be very narrow or even absent. Frena are small folds of mucous membrane that connect the lips or cheeks to the alveolar mucosa and gingiva. A high frenal attachment, inserting close to or at the gingival margin and potentially crossing the MGJ, can sometimes exert a pull that might influence the gum line, especially if the band of attached gingiva is minimal. This is an anatomical variation that dental professionals observe.
It’s also worth noting that on the palate (the roof of your mouth), there is typically no alveolar mucosa and therefore no distinct MGJ in the same way as on the facial or buccal (cheek) aspects. The palatal tissue is mostly keratinized masticatory mucosa, firmly attached to the bone, similar to attached gingiva.
A Testament to Oral Design
The mucogingival junction is a fascinating example of the body’s intricate and functional design. This often-overlooked line plays a crucial role in the everyday activities of eating, speaking, and maintaining oral health. It elegantly solves the biomechanical problem of needing a tough, stable tissue around the teeth while also requiring a flexible, movable lining for the rest of the oral cavity. Understanding its anatomy helps us appreciate the complexity hidden within even the seemingly simplest parts of our bodies. While you may not think about it daily, the MGJ is a silent guardian, diligently performing its duties to ensure your oral environment functions smoothly and efficiently.
Next time you’re brushing your teeth, take a moment to (gently!) pull back your lip and see if you can spot this subtle yet significant boundary. It’s a small reminder of the wonderfully complex biological systems at work within us, each component, no matter how unassuming, playing its part in the grand scheme of our well-being.