Deep within each of your teeth, hidden beneath the hard, protective layers of enamel and dentin, lies a vital, living core known as the dental pulp. Often referred to as the “heart” or “nerve” of the tooth, the pulp is a soft tissue that plays a crucial role in a tooth’s life, from its development to its everyday function and sensation. Understanding this inner sanctum is key to appreciating why looking after your teeth is so important, as the health of the pulp is directly linked to the overall health and longevity of your tooth.
Peeking Inside: What is Tooth Pulp?
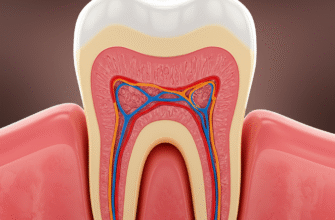
Imagine your tooth as a tiny fortress. The outer enamel is the strong, visible wall, and beneath it lies the dentin, a slightly softer, yellowish layer that makes up the bulk of the tooth structure. At the very center of this fortress is the pulp chamber, a hollow space within the crown (the part of the tooth you see above the gumline). This chamber extends downwards through the roots of the tooth via narrow channels called root canals, which reach towards the tip of each root. It is within this protected space – the pulp chamber and root canals – that the dental pulp resides.
The pulp itself is a complex mix of several components, each with a specific job:
- Blood Vessels: Tiny arteries and veins weave their way into the pulp, bringing a constant supply of nutrients and oxygen. This vascular network is essential for keeping the tooth’s cells alive and functioning. It also carries away waste products.
- Nerves: The pulp is rich in nerve fibers. These nerves are responsible for the sensations your tooth can feel, such as changes in temperature (hot and cold) and pressure. Crucially, they are also the source of pain signals when something is wrong, acting as an alarm system.
- Connective Tissue: This is the “stuffing” that holds everything together, providing structure and support for the blood vessels and nerves within the pulp. It’s made up of cells like fibroblasts and an extracellular matrix.
- Specialized Cells (Odontoblasts): Lining the outer edge of the pulp, right next to the dentin, are highly specialized cells called odontoblasts. These cells are responsible for producing dentin. While their primary role is during tooth formation, they can also produce reparative dentin later in life if the tooth experiences irritation.
- Other Cells: The pulp also contains various other cells, including immune cells like macrophages and lymphocytes, which play a role in defending against infection.
The Many Jobs of the Pulp
The dental pulp isn’t just passively sitting there; it’s actively working throughout the life of your tooth, performing several vital functions.
Sensation Central
Perhaps the most commonly known function of the pulp is its sensory role. The nerves within the pulp are highly sensitive. When you sip a hot coffee or bite into ice cream, it’s the pulp that registers that temperature. This sensitivity isn’t just for kicks; it’s a protective mechanism. If you experience a sudden, sharp pain, it’s often the pulp signaling that something is amiss – perhaps a cavity is getting too close, or there’s a crack in the tooth. This early warning system can prompt you to seek dental attention before a problem becomes more severe.
Keeping Things Alive: Nutrition and Hydration
The blood supply to the pulp is critical for maintaining the vitality of the tooth, particularly the dentin. While enamel is acellular (contains no living cells), dentin is a living tissue permeated by microscopic tubules that extend from the pulp. The pulp provides the necessary nutrients and moisture to keep the dentin healthy and resilient. A tooth with a healthy pulp is generally stronger and less brittle than a tooth that has had its pulp removed (for example, after a root canal treatment).
The Tooth Builder (Initially)
During the development of a tooth, the pulp, specifically its odontoblast cells, plays a primary role in forming the dentin. As the tooth grows and erupts, odontoblasts lay down successive layers of dentin, shaping the tooth from the inside out. Once the tooth is fully formed, this primary dentin formation largely ceases, but the odontoblasts remain, capable of further action if needed.
A Little Bit of Defense and Repair
The pulp has a limited capacity to defend itself and repair damage. When faced with mild irritation, such as a slowly progressing cavity or minor wear, the odontoblasts can be stimulated to produce what’s called tertiary dentin (or reparative dentin). This new layer of dentin is laid down on the pulp chamber wall, directly beneath the site of irritation, effectively creating a thicker barrier to protect the pulp. The pulp also contains immune cells that can help fight off invading bacteria, although this defense mechanism can be overwhelmed if the bacterial invasion is too aggressive or prolonged.
Persistent tooth pain, especially if it’s severe, wakes you up at night, or is accompanied by swelling in the gums or face, often indicates an issue with the pulp that requires professional dental attention. Ignoring such symptoms can sometimes lead to more complex problems, including infection. It’s generally a good idea to consult with a dental professional if you experience ongoing or concerning dental discomfort.
When the Pulp Cries Out: Problems and Symptoms
Despite its protected location, the pulp can become irritated, inflamed, or infected. This condition is generally known as pulpitis. Pulpitis can be reversible if the irritation is mild and caught early, or irreversible if the damage is too severe for the pulp to recover.
Common causes of pulp problems include:
- Deep Dental Decay (Cavities): This is the most common culprit. Bacteria in plaque produce acids that eat through enamel and dentin. If decay reaches the pulp, bacteria can invade, leading to inflammation and infection.
- Cracks or Fractures: A crack in the tooth can create a pathway for bacteria to reach the pulp, even if the crack isn’t visible to the naked eye.
- Trauma or Injury: A blow to the tooth, from a fall or sports injury, can damage the pulp directly, sometimes even severing its blood supply.
- Repeated Dental Procedures: Multiple fillings or other treatments on the same tooth can, over time, cause stress and inflammation in the pulp.
- Severe Gum Disease (Periodontitis): In advanced cases, gum disease can progress down the side of the tooth root, potentially allowing bacteria to enter the pulp via accessory canals near the root tip.
- Bruxism (Teeth Grinding): Constant, heavy forces from grinding or clenching can traumatize the pulp over time.
Symptoms that might indicate a pulp problem can vary in intensity and type, but often include:
- Spontaneous Pain: Pain that occurs without any obvious trigger, and can be throbbing or aching.
- Lingering Sensitivity: Pain or sensitivity to hot or cold temperatures that lasts for more than a few seconds after the stimulus is removed.
- Pain on Biting or Chewing: Sharp pain or discomfort when pressure is applied to the tooth.
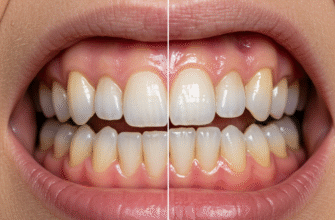
- Tooth Discoloration: A tooth may appear darker (greyish or brownish) if the pulp has died or is dying.
- Swelling or Tenderness: Swelling in the gums near the affected tooth, or even facial swelling, can indicate an infection spreading from the pulp.
- A Pimple-like Bump (Fistula) on the Gum: This can be a sign that an abscess (a collection of pus) associated with an infected pulp is trying to drain.
It’s important to note that sometimes, a pulp can die without causing significant pain, especially if the process is slow. This is why regular dental check-ups are so valuable, as a dentist can sometimes spot signs of a non-vital tooth even if you aren’t experiencing obvious symptoms.
What Can Be Done? Approaches to Pulp Issues
When the pulp is in trouble, the primary goals of dental treatment are to alleviate any discomfort, eliminate infection if present, and, whenever possible, save the natural tooth. The specific approach will depend on whether the pulpitis is considered reversible or irreversible, and the overall condition of the tooth.
For Irreversible Pulpitis or Pulp Necrosis (Dead Pulp)
If the pulp is irreversibly inflamed or has died and become infected, it cannot heal itself. In these situations, there are generally two main treatment paths:
- Root Canal Treatment (Endodontic Therapy): This is a common and highly successful procedure designed to save the tooth. During a root canal, the dentist or endodontist (a root canal specialist) carefully removes the inflamed or infected pulp tissue from the pulp chamber and root canals. The inside of the tooth is then thoroughly cleaned, disinfected, shaped, and finally filled and sealed with a biocompatible material. After a root canal, the tooth will no longer have a living pulp and will lose its ability to feel hot or cold, but it can continue to function normally for many years. Often, a crown is recommended afterwards to protect the treated tooth.
- Extraction: If the tooth is too severely damaged to be restored, if there’s extensive bone loss around it, or if a patient opts against root canal treatment, then extracting (removing) the tooth may be the only alternative. If a tooth is extracted, options for replacing it, such as a bridge, implant, or partial denture, are usually discussed.
For Reversible Pulpitis
If the pulp inflammation is mild and the cause can be removed, the pulp may be able to recover. For instance, if a small cavity is causing sensitivity, removing the decay and placing a filling might be all that’s needed. The sensitivity should then subside. In some cases where decay is very close to the pulp but hasn’t quite reached it, a dentist might place a sedative dressing or a special liner (pulp capping) under the filling to help calm the pulp and encourage the formation of reparative dentin.
Protecting Your Pulp: Keeping Teeth Healthy
The best way to deal with pulp problems is to prevent them from happening in the first place. Protecting your pulp means protecting your overall tooth health. Here are some key strategies:
- Practice Excellent Oral Hygiene: Brush your teeth thoroughly twice a day with fluoride toothpaste and floss daily. This helps remove plaque and food debris, preventing cavities that can eventually threaten the pulp.
- Regular Dental Check-ups and Cleanings: Visit your dentist regularly (as recommended for your individual needs). Professional cleanings remove hardened plaque (tartar) that you can’t remove at home, and check-ups allow for early detection and treatment of cavities or other issues before they become serious pulp problems.
- Eat a Balanced Diet: Limit sugary and acidic foods and drinks, as these contribute to tooth decay.
- Wear a Mouthguard: If you play contact sports or engage in activities where your teeth could be injured, wear a custom-fitted mouthguard to protect against trauma.
- Address Teeth Grinding (Bruxism): If you grind or clench your teeth, especially at night, talk to your dentist. They may recommend a nightguard to protect your teeth from excessive wear and stress.
- Don’t Ignore Symptoms: If you experience tooth sensitivity, pain, or notice any changes in your mouth, see your dentist promptly. Early intervention is key.
Your dental pulp is a small but incredibly important part of your oral anatomy. It’s the life force within your tooth, responsible for sensation, nutrition, and even some defense. By understanding its role and taking good care of your teeth, you can help ensure your pulp stays healthy, allowing your natural teeth to serve you well for a lifetime. When issues do arise, modern dentistry offers effective ways to address pulp problems, often preserving the tooth and restoring comfort and function.