While a bright smile showcases the crowns of our teeth, there’s an entire unseen world beneath the gumline that provides the crucial foundation: the tooth root system. This intricate network is far more than just a simple peg holding a tooth in place. It’s a dynamic, living structure responsible for anchorage, sensation, and nourishment. Understanding its various components helps us appreciate the complexity of even a single tooth and the engineering marvel it represents within our jaws.
Core Structures: The Building Blocks of the Root
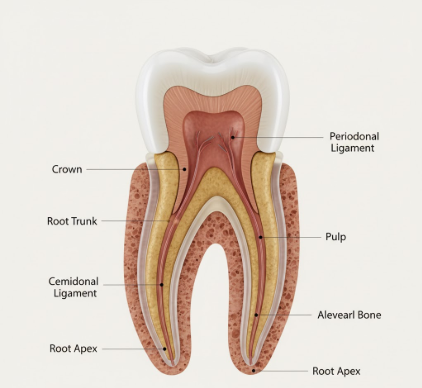
Cementum: The Root’s Protective Outer Garment
Covering the entire outer surface of the root is a specialized, calcified tissue called
cementum. Think of it as the root’s version of enamel, though it’s not nearly as hard. Its primary job is to provide a surface for the fibers of the periodontal ligament (which we’ll explore shortly) to attach, effectively anchoring the tooth into its bony socket. Cementum is continually, albeit slowly, deposited throughout life, a process that can help compensate for minor tooth wear or facilitate slight adjustments in tooth position. There are generally two main types: acellular cementum, which is formed first and covers roughly the cervical two-thirds of the root, and cellular cementum, typically found on the apical third and in areas where roots divide (furcations), which forms more rapidly and contains cells called cementocytes.
Dentin: The Resilient Core
Beneath the thin layer of cementum lies
dentin, which forms the substantial bulk of the root structure, just as it forms the bulk of the tooth’s crown underneath the enamel. Dentin is a hard, dense, yellowish-white tissue, more mineralized than bone but softer and more elastic than enamel. Its most characteristic feature is its microscopic structure, composed of countless tiny channels called dentinal tubules. These tubules radiate outwards from the central pulp cavity towards the cementum. Each tubule contains fluid and a long, slender cytoplasmic process from an odontoblast cell, whose body lines the pulp cavity. This tubular network is the reason why, if cementum is lost and dentin becomes exposed, teeth can become sensitive to temperature changes or certain foods.
The Pulp Canal: Lifeline Through the Root
Running like a central corridor through the dentin in each root is the
pulp canal, often referred to simply as the root canal. This narrow channel is a continuation of the pulp chamber, which is located in the crown of the tooth. The pulp canal extends from the floor of the pulp chamber down to the very tip, or apex, of the root. It’s not an empty space; rather, it’s precisely shaped to house the vital pulp tissue. The morphology of pulp canals can be surprisingly complex, varying in shape, size, and number even within a single tooth, presenting unique anatomical landscapes.
Pulp Tissue: The Living Heart
Housed within the protective confines of the pulp chamber and the pulp canal(s) is the
pulp tissue. This is the living, innermost part of the tooth, a soft, gelatinous connective tissue. It’s a rich environment, containing an intricate network of blood vessels (arterioles and venules), lymphatic vessels, nerves, and specialized cells, including odontoblasts (responsible for dentin formation) and fibroblasts. The blood vessels provide essential nutrients and oxygen to keep the tooth alive and responsive, while the nerves are primarily sensory, transmitting signals such as pain, temperature, and pressure, thereby acting as a biological alarm system for the tooth.
Apical Foramen: The Gateway at the Tip
At the very end, or apex, of each root tip is a tiny, crucial opening called the
apical foramen. This is the main portal through which the blood vessels, nerves, and lymphatic drainage from the surrounding jawbone enter and exit the pulp canal system. It’s a critical juncture, directly connecting the tooth’s internal, living environment with the rest of the body’s circulatory and nervous systems. While usually there’s one main foramen, it’s not uncommon to find multiple smaller openings, known as accessory foramina or an apical delta, especially in mature teeth, creating a more complex network at the root’s terminus.
The Root’s Essential Support Network
The root itself is just one part of a sophisticated system designed to keep the tooth firmly in place and functioning correctly. Its immediate neighbors are just as important.
Periodontal Ligament (PDL): The Tooth’s Suspension System
While not technically part of the tooth root itself, the
periodontal ligament (PDL) is an absolutely indispensable component of the tooth root system. The PDL is a specialized, highly vascular and cellular connective tissue composed of countless tiny collagenous fibers. These fibers are precisely arranged to surround the root, effectively suspending the tooth in its bony socket. One end of these fibers (Sharpey’s fibers) embeds into the cementum of the root, and the other end embeds into the alveolar bone. This arrangement doesn’t just hold the tooth; it acts like a sophisticated shock absorber, cushioning the tooth and bone against the considerable forces of chewing and biting. The PDL also contains nerves that provide vital sensory information about tooth movement, pressure, and pain, helping to modulate bite force and protect the tooth from excessive loads. It also plays roles in tooth eruption and maintaining the physiological tooth position.
The periodontal ligament is a truly remarkable tissue. It not only anchors the tooth securely but also allows for slight physiological movement, which is essential for distributing and dissipating chewing forces. Furthermore, it contains a rich supply of cells capable of forming new cementum and bone, contributing to ongoing repair and adaptation processes throughout an individual’s life, responding to functional demands.
Alveolar Bone: The Snug Socket
The
alveolar bone, also known as the alveolar process, is the specialized part of the jawbone (either the maxilla in the upper jaw or the mandible in the lower jaw) that forms the bony sockets, or alveoli, which house the tooth roots. The integrity of this bone is crucial for tooth support. The PDL fibers embed directly into this bone on one side and into the root’s cementum on the other, creating a strong yet dynamic fibrous joint known as a gomphosis. The alveolar bone is constantly undergoing remodeling – breaking down and rebuilding – in response to the functional stresses placed upon it by the teeth. Its health and density are critical for the long-term stability and retention of the teeth.
Not All Roots Are Created Equal: Embracing Variation
The fundamental components of the tooth root system are consistent across all teeth, but their specific configuration, number, and complexity can vary dramatically. This anatomical diversity is a key aspect of dental science and has practical implications for how teeth function and are cared for.
Number of Roots: From Solo Acts to Multi-Rooted Ensembles
Teeth are often classified by the number of roots they possess, which generally correlates with their size and functional demands:
- Single-rooted teeth: Typically, the anterior teeth (incisors and canines) and most premolars (bicuspids) in both arches have a single root. This simpler structure is well-suited for their primary functions of cutting, piercing, and tearing food.
- Multi-rooted teeth: Molars, designed for grinding and heavy mastication, almost always have multiple roots to provide a broader base for increased stability and resistance to occlusal forces. Upper molars commonly have three roots (two buccal, or cheek-side, and one palatal, or roof-of-the-mouth-side). Lower molars usually have two robust roots (one mesial, towards the front of the mouth, and one distal, towards the back). Some upper premolars, particularly the first premolars, can also be bi-rooted or even occasionally tri-rooted.
The Intricacies of Canal Systems Within Roots
The complexity doesn’t end with the number of roots. The internal anatomy, specifically the number and configuration of root canals within each root, can be highly variable. It’s a common misconception that one root equals one canal. For instance, the mesial root of a lower molar very frequently contains two distinct canals. These canals might remain separate for their entire length, or they could merge to exit through a single apical foramen, or even branch and rejoin multiple times. Mandibular incisors, though single-rooted, can sometimes present with two canals. Understanding this internal ‘plumbing’ is vital.
Accessory and Lateral Canals: The Hidden Pathways
Adding further layers to the root canal system’s complexity are
lateral canals and
accessory canals. Lateral canals are small channels that typically branch off the main root canal, often at a right angle, and extend horizontally or obliquely to the outer surface of the root, connecting with the periodontal ligament. Accessory canals are similar but are usually found in the apical third of the root, sometimes forming a delta-like pattern of multiple tiny openings near the main apical foramen. These canals are formed during tooth development when blood vessels supplying the developing pulp become entrapped. While normal anatomical features, they can become significant if the main pulp becomes compromised, as they can act as pathways for irritants to reach the periodontal tissues.
Roots are rarely the perfectly straight, symmetrical cones often depicted in simplified diagrams. They frequently exhibit varying degrees of curvature, sometimes quite pronounced, along their length. They can twist, taper dramatically, or be broad and flat. Roots can also be exceptionally long or surprisingly short. In multi-rooted teeth, the roots might splay widely or be closely bunched. Sometimes, roots can even be fused together, either partially or completely (a condition known as concrescence if it involves cementum fusion, or fusion if it occurs during dentin development). These anatomical nuances are highly significant, influencing how forces are distributed and how dental professionals approach any procedures involving the root structure.
Why Understanding the Root System Matters
The tooth root system, though largely hidden from everyday view, is absolutely fundamental to our oral health and overall masticatory function. Its intricate and robust design ensures that our teeth can withstand the daily rigors of biting, tearing, and grinding food, while also providing vital sensory feedback to the brain. The health of the surrounding gums and the supporting alveolar bone is inextricably linked to the integrity of the root and its periodontal ligament attachment.
A sound and well-supported root system provides the stable foundation necessary for a tooth to perform its designated duties effectively and comfortably throughout an individual’s life. When one considers the significant forces involved in mastication – forces that can be quite substantial – the precise engineering of the root’s shape, number, and its anchoring mechanism within the jawbone becomes truly impressive. Furthermore, the rich nerve supply within the root canals serves as an invaluable early warning system, capable of signaling potential issues such as advancing decay, cracks, or inflammation, which might otherwise go unnoticed until more significant or irreversible damage has occurred. This detailed anatomical understanding profoundly informs various dental practices, enabling professionals to provide care that is precisely tailored to the unique and often complex anatomy of each individual tooth and its supporting structures.
The Unseen Anchor: A Complex Marvel
In conclusion, the tooth root system is far more than just a passive anchor holding a tooth in the jaw. It is a dynamic, sophisticated biological structure comprising specialized hard tissues like cementum and dentin, a vital pulp tissue providing nourishment and sensation through often intricate canal networks, and a critical, resilient connection to the jawbone via the periodontal ligament. The wide-ranging variations in root number, internal canal configuration, curvature, and overall form underscore the remarkable adaptability and inherent complexity of human dentition. By appreciating these often-overlooked components, we gain a deeper and more comprehensive understanding of overall dental health, the functional demands placed on our teeth, and the incredible natural engineering that allows them to serve us so well.