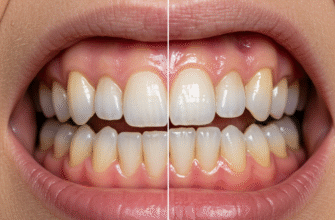
It’s a common belief, almost a sigh of relief for many: once a tooth gets a dental crown, it’s like it’s been encased in an impenetrable fortress, safe from the dreaded sugar bugs that cause cavities. People often think that the porcelain or metal shield is the ultimate defense, meaning no more worries about decay for that particular tooth. Unfortunately, this is a significant misconception, and believing it can lead to some rather unpleasant and unexpected dental issues down the line. While a crown itself is indeed made of materials that cannot decay, the natural tooth structure hiding underneath, especially at the edges, remains vulnerable.
Understanding What a Dental Crown Does (and Doesn’t Do)
Before we dive into how cavities can form under these protective caps, let’s quickly recap what a dental crown is. A crown, sometimes called a cap, is a custom-made covering that fits over the entire visible portion of a tooth, right down to the gum line. Dentists recommend crowns for various reasons: to restore a tooth that’s significantly damaged by decay or fracture, to protect a weak tooth from breaking, to cover a tooth after a root canal procedure, to hold a dental bridge in place, or even for cosmetic enhancements.
The crown acts like a helmet, reinforcing the tooth and restoring its shape, size, strength, and appearance. Materials like porcelain, ceramic, metal alloys, or a combination (porcelain-fused-to-metal) are used, all of which are highly resistant to the bacterial acids that cause tooth decay. So,
the crown material itself is safe from cavities. The problem, however, lies with what’s underneath and around it.
The Achilles’ Heel: Where Crown Meets Tooth
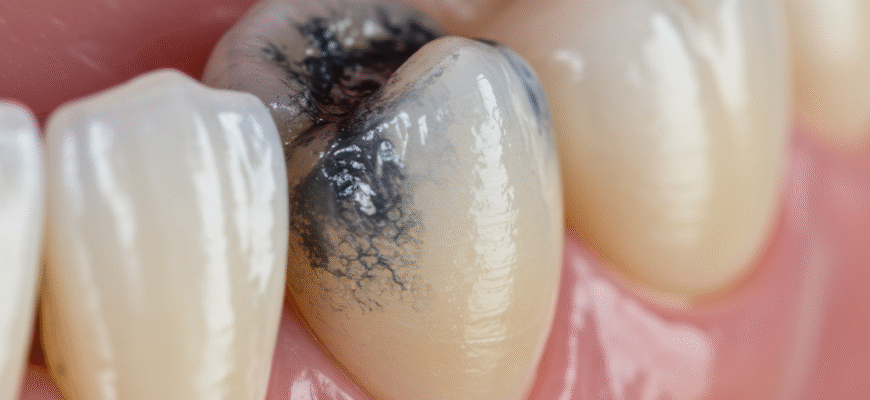
The most vulnerable area for a crowned tooth is the
margin – the line where the edge of the crown meets the surface of your natural tooth. This junction is the critical point. If this seal isn’t perfect, or if it becomes compromised over time, it creates an opportunity for bacteria to sneak in. Think of it like a lid on a jar; if the lid isn’t sealed tightly all the way around, what’s inside can still spoil.
Bacteria aren’t particularly discerning; they’ll happily colonize any tooth surface they can access, especially if there’s a food supply (sugars and starches) available. Plaque, that sticky film of bacteria, can accumulate along this margin just like it does on any other tooth surface. If not diligently removed, the bacteria in the plaque will produce acids, and these acids will begin to eat away at the exposed natural tooth structure right at the edge of the crown. This is how a new cavity, often called recurrent decay or secondary decay, can start.
Important Reminder: A dental crown does not make a tooth immune to decay. The natural tooth structure beneath the crown, particularly at the margin where the crown meets the tooth, can still develop cavities. Consistent and thorough oral hygiene, along with regular dental check-ups, are essential for the long-term health of crowned teeth.
Why Do These Undercover Cavities Occur?
Several factors can contribute to decay forming under or around a dental crown:
- Inadequate Oral Hygiene: This is the most common culprit. If brushing and flossing aren’t effectively removing plaque from the gumline and the crown margins, bacteria will thrive. It’s crucial to brush carefully around the base of the crown and to floss between the crowned tooth and its neighbors.
- Dietary Habits: A diet high in sugary and acidic foods and drinks fuels the bacteria that cause cavities. These bacteria produce more acid, increasing the risk of decay, even around well-placed crowns.
- Cement Washout: The dental cement used to bond the crown to the tooth isn’t permanent. Over many years, it can gradually wash out or dissolve, especially if exposed to oral fluids. This can create tiny gaps between the crown and the tooth, providing an entry point for bacteria.
- Ill-Fitting Crown: If a crown doesn’t fit perfectly from the start, there might be small gaps or ledges at the margin. These imperfections can trap plaque and make cleaning difficult, leading to decay. This is less common with modern dental techniques but can happen.
- Gum Recession: As we age, or due to gum disease, our gums can recede. If the gums recede around a crowned tooth, they can expose the root surface of the tooth, which is softer and more susceptible to decay than enamel. The margin of the crown might then be sitting on this vulnerable root surface.
- Pre-existing Conditions: If a tiny bit of decay wasn’t completely removed before the crown was placed (though dentists are very careful about this), it could potentially continue to grow. More commonly, a new cavity forms at the margin.
- Age of the Crown: Crowns don’t last forever. The average lifespan is typically 10-15 years, but this varies greatly depending on oral hygiene, diet, biting forces (like grinding or clenching), and the material of the crown. As crowns age, the risk of cement failure or microleakage can increase.
The Stealthy Nature of Cavities Under Crowns
One of the tricky things about decay under a crown is that it can be quite stealthy. Because the crown covers the tooth, you can’t see what’s happening underneath. Often, these cavities don’t cause any pain or sensitivity in their early stages. By the time symptoms do appear, the decay might already be quite extensive.
Possible signs that might indicate a problem include:
- Sensitivity: You might notice sensitivity to hot, cold, or sweet foods and drinks around the crowned tooth.
- Pain or Ache: A persistent dull ache or sharp pain when biting down could be a sign.
- Bad Breath or Unpleasant Taste: Decay can sometimes lead to a foul odor or taste originating from the affected area.
- Loose Crown: If the underlying tooth structure is compromised by decay, the crown may become loose or even fall off.
- Discoloration: Sometimes, a dark line or discoloration might become visible at the margin of the crown, though this isn’t always indicative of decay.
- Gum Inflammation: Swollen or bleeding gums around the crown could signal an issue.
However, it’s also very common for there to be
no noticeable symptoms at all, especially in the early stages. This is why regular dental check-ups are so vital.
How Dentists Detect These Hidden Cavities
Dentists have a few key tools and techniques to check for decay under existing crowns:
- Clinical Examination: The dentist will carefully examine the margins of the crown with a dental explorer (a sharp, pointed instrument). They are looking for any softness, stickiness, or gaps that could indicate decay. They’ll also check the surrounding gum tissue.
- Dental X-rays (Radiographs): X-rays are invaluable for detecting cavities under crowns. A specific type of X-ray called a bitewing can often show decay starting at the margin and progressing under the crown. However, if the crown is made of metal, the metal can sometimes obscure the view of decay directly underneath it on an X-ray. In such cases, changes in the bone or root area might hint at a problem.
- Patient-Reported Symptoms: Your dentist will listen carefully to any symptoms you’ve been experiencing, like sensitivity or pain, as these can be important clues.
Regular dental visits, typically every six months (or as recommended by your dentist), allow for early detection of such problems. The sooner a cavity under a crown is found, the simpler the treatment is likely to be.
Prevention: Your Best Strategy
The good news is that you can take proactive steps to significantly reduce the risk of getting a cavity under your dental crown. Prevention largely mirrors how you’d prevent cavities in any other tooth:
- Meticulous Brushing: Brush at least twice a day for two minutes, paying special attention to the gum line where the crown meets the tooth. Use a soft-bristled toothbrush and fluoride toothpaste. Consider an electric toothbrush, as many find them more effective at plaque removal.
- Daily Flossing: Flossing is non-negotiable! It’s the only way to effectively clean the tight spaces between teeth and right up to the margin of the crown. Gently slide the floss up and down, curving it around the base of the crown. Floss threaders or interdental brushes can be helpful for cleaning around crowns and bridges.
- Antiseptic Mouthwash: Rinsing with an antiseptic mouthwash can help reduce bacteria in your mouth, but it’s a supplement to, not a replacement for, brushing and flossing.
- Balanced Diet: Limit your intake of sugary snacks, sticky candies, and acidic beverages (like sodas and sports drinks). If you do consume them, try to do so with meals rather than sipping or snacking throughout the day, and rinse your mouth with water afterward.
- Regular Dental Check-ups and Cleanings: Visit your dentist and hygienist as recommended. Professional cleanings remove plaque and tartar that you can’t remove at home, and regular exams help catch problems early.
- Address Grinding or Clenching: If you grind or clench your teeth (bruxism), discuss it with your dentist. This can put excessive stress on crowns and potentially compromise their seal over time. A nightguard might be recommended.
If decay is detected under a crown, the treatment approach will depend on the extent and location of the cavity.
- Minor Decay at an Accessible Margin: In some rare cases, if the decay is very small and located at an easily accessible part of the crown’s margin, your dentist *might* be able to repair it without removing the crown. This is not common.
- Crown Removal and Replacement: More often, the crown will need to be removed to allow the dentist to fully access and clean out all the decay. Once the decay is removed, the tooth will be assessed. If there’s enough healthy tooth structure remaining, a new crown will be made. The old crown usually cannot be reused because it may be damaged during removal or may no longer fit properly after the decay is treated.
- Root Canal Treatment: If the decay has reached the pulp (the inner nerve and blood vessel chamber) of the tooth, a root canal treatment may be necessary before a new crown can be placed.
- Tooth Extraction: In severe cases, if the decay is very extensive and has compromised too much of the tooth structure, or if there’s a fracture, the tooth might not be salvageable and may need to be extracted. This is, of course, the outcome everyone wants to avoid.
So, while dental crowns are fantastic restorations that can save teeth and improve smiles for many years, they don’t grant immunity from future problems. The underlying tooth is still there, and it still needs your diligent care. Busting the myth that you can’t get cavities under crowns is the first step to ensuring your crowned teeth stay healthy for as long as possible. Remember, that crown is a partnership between your dentist’s skill and your ongoing commitment to oral hygiene.