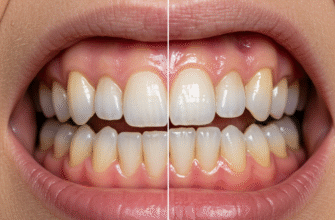
Okay, let’s dive straight into the fascinating world beneath your gumline. Most of us think about the shiny white enamel when we picture our teeth, and that’s fair – it’s the part we see every day. But a tooth is a complex structure, and its hidden portions are just as crucial for its health and longevity. Deep within the jawbone, the roots of our teeth are anchored, providing stability for chewing and speaking. These roots aren’t bare; they have their own specialized covering, a remarkable tissue that plays a vital role not just in anchoring but also in mending.
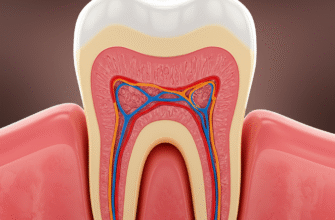
To truly appreciate how teeth can mend themselves, even in small ways, we need a quick look at their basic anatomy. The crown, the visible part, is coated in super-hard enamel. Beneath that lies dentin, a yellowish, bone-like material that forms the bulk of the tooth and extends down into the root. At the very core is the pulp, containing nerves and blood vessels. Now, when we move down from the crown to the root, the enamel gives way. Instead, the root dentin is covered by a different, yet equally important, layer. This layer is called cementum.
Meet Cementum: The Root’s Unsung Hero
Cementum is a specialized, calcified connective tissue that forms a thin layer over the anatomical root of a tooth. Think of it as the enamel of the root, though its composition and properties are quite different. While enamel is incredibly hard and mostly inorganic, cementum is more akin to bone in its makeup, containing about 45-50% inorganic mineral (hydroxyapatite) and 50-55% organic matter (primarily collagen) and water. This composition gives it a certain degree of resilience and, crucially, the ability to undergo repair and remodeling throughout life, albeit to a lesser extent than bone.
The cells responsible for forming cementum are called cementoblasts. These cells line the surface of the cementum, particularly near the periodontal ligament – the fibrous tissue that connects the tooth root to the alveolar bone of the jaw. As cementum is laid down in layers, some cementoblasts can become entrapped within the matrix they produce. Once entrapped, they are referred to as cementocytes, residing in small spaces called lacunae, much like osteocytes in bone.
Types of Cementum and Their Functions
Not all cementum is the same. There are primarily two types, distinguished by the presence or absence of cells within their matrix and their location on the root:
Acellular Cementum (Primary Cementum): This type is the first to be formed and covers roughly the cervical two-thirds of the root (the part closest to the crown). As its name suggests, it does not contain any cells within its calcified matrix. It is formed more slowly than cellular cementum and its collagen fibers are typically well-organized, running parallel to the root surface. Its main function is anchorage, providing a firm attachment for the fibers of the periodontal ligament.
Cellular Cementum (Secondary Cementum): This type is formed after the tooth has erupted and is in function. It is mainly found on the apical third of the root (the tip) and in the areas between roots of multi-rooted teeth (furcation areas). Cellular cementum contains cementocytes trapped within its matrix. It is formed more rapidly than acellular cementum and is less calcified. Its primary role is adaptive; it can be deposited in layers throughout life in response to wear, tooth movement, or to repair minor damage. This is where its reparative capabilities truly shine.
Whispers of Wear: How Minor Root Damage Can Happen
Our teeth are constantly subjected to forces. Chewing, slight movements, and even some dental procedures can, over time, lead to microscopic areas of damage on the root surface. This isn’t necessarily a cause for alarm in its initial, minor stages, as the body has mechanisms to cope. Some common scenarios where minor root surface resorption (a process where tiny bits of the root are broken down and removed) might occur include:
- Orthodontic Treatment: The controlled forces applied during orthodontic treatment (like braces) intentionally cause remodeling of the bone and can sometimes lead to very slight, localized root resorption. This is usually minimal and clinically insignificant, often followed by repair.
- Occlusal Trauma: If teeth are not meeting correctly (malocclusion) or if there are habits like clenching or grinding (bruxism), excessive forces can be placed on certain teeth. This can sometimes trigger a minor resorptive response on the root surface.
- Slight Physical Trauma: A minor knock to a tooth, not severe enough to cause fracture or dislocation, might still cause microscopic injury at the root level.
- Physiological Tooth Movement: Teeth naturally undergo minute shifts and movements throughout life, which can involve minor remodeling of both bone and cementum.
- Idiopathic Resorption: Sometimes, small areas of resorption occur without a clearly identifiable cause.
It’s important to distinguish this minor, often microscopic, resorption from more aggressive forms of root resorption that are pathological and require dental intervention. We are focusing here on the body’s ability to handle small-scale incidents.
The Healing Touch: Cementum’s Repair Mechanism
When a small area of the cementum or even the underlying root dentin experiences minor resorption, the body doesn’t just leave it damaged. The cementoblasts, those industrious cells we mentioned earlier, play a pivotal role in the repair process. This natural mending is a fascinating example of the body’s inherent ability to maintain tissue integrity.
The process generally involves a sequence of cellular events. Once the cause of the minor resorption is removed or ceases (for example, orthodontic forces are adjusted, or slight trauma heals), the environment becomes conducive for repair. Specialized cells will clean up the damaged area. Following this, cementoblasts are signaled to become active.
Step-by-Step: How Cementum Patches Things Up
The repair sequence, though complex at a cellular level, can be broadly understood as follows:
- Resorption Ceases: The stimulus causing the resorption must stop for repair to begin effectively.
- Recruitment and Activation of Cementoblasts: Precursor cells differentiate into active cementoblasts, or existing quiescent cementoblasts are activated. These cells migrate to the site of the defect on the root surface.
- Deposition of Cementoid: The activated cementoblasts begin to lay down an organic matrix, primarily composed of collagen fibers and ground substance. This unmineralized new layer is called cementoid.
- Mineralization: The cementoid subsequently mineralizes, incorporating calcium and phosphate ions to become hard cementum. This new layer of cementum effectively fills in the resorbed area, restoring the contour of the root surface.
- Re-establishment of Attachment: If the periodontal ligament fibers were disrupted by the resorption, new fibers will embed into the newly formed cementum, restoring the tooth’s attachment to the surrounding bone. This new cementum is often of the cellular type, capable of being laid down more quickly to facilitate repair.
This repair cementum, sometimes called “reparative cementum,” aims to resurface the defect and re-establish a functional periodontal ligament attachment. The success and extent of this repair depend on several factors, including the size of the defect and the overall health of the surrounding tissues.
Cementum repair is a dynamic biological process. Active cementoblasts are crucial for depositing new cementum matrix, which then mineralizes to mend small defects on the tooth root. This process highlights the living nature of tissues supporting our teeth.
Influences on the Mend: What Affects Cementum Repair?
While cementum possesses this remarkable capacity for repair, its effectiveness isn’t absolute and can be influenced by various factors. The body’s ability to mend these minor root issues is a delicate balance.
Size and Nature of the Defect: The most significant factor is the extent of the damage. Cementum repair is generally effective for small, shallow areas of resorption. Larger defects, or those that penetrate deeply into the dentin, may not be fully repaired by cementum alone and might require professional dental intervention. If the damage is ongoing or caused by a persistent issue like untreated infection, the repair process will be hampered.
Systemic Health: A person’s overall health can play a role. Conditions that affect general healing processes or bone metabolism might also influence the efficiency of cementum repair. Good nutrition, providing the necessary building blocks for tissue regeneration, is also beneficial.
Local Tissue Health: The health of the surrounding periodontal tissues, including the gums and periodontal ligament, is critical. Inflammation or infection in these areas can hinder or prevent cementum repair. A healthy, non-inflamed environment is conducive to the proper functioning of cementoblasts.
Presence of Cementoblasts: For repair to occur, there must be a viable source of cementoblasts or their precursor cells near the damaged area. If these cells are compromised or absent, repair will be limited.
Blood Supply: Like any healing process, an adequate blood supply to the area is necessary to deliver nutrients and cells required for repair.
It’s crucial to understand that cementum’s self-repair is primarily for minor, superficial root surface issues. It is not a solution for cavities, advanced gum disease, significant root fractures, or extensive root resorption. These conditions require professional diagnosis and treatment from a dentist.
The repair process is also generally slower than bone remodeling. While effective, it is a gradual mending. The focus is on restoring surface integrity and attachment, not on regenerating large volumes of lost tooth structure.
Nurturing Your Tooth’s Innate Defenses
Understanding that our teeth have these inherent, albeit limited, repair mechanisms underscores the importance of supporting our body’s natural processes. While cementum can patch up minor wear and tear on the roots, it can’t do it all, especially in the face of persistent neglect or significant damage.
The best way to support this natural mending capability is to minimize the damage in the first place and maintain a healthy oral environment. Good oral hygiene practices, such as regular and proper brushing and flossing, are paramount. These actions help remove plaque, a biofilm of bacteria that can lead to gum inflammation (gingivitis) and, if left unchecked, more severe periodontal disease. Chronic inflammation around the tooth roots creates an unfavorable environment for cementoblasts and can even promote resorption rather than repair.
Regular dental check-ups also play a role, not by directly enhancing cementum repair, but by identifying and addressing issues that could lead to root damage or hinder natural repair processes. For instance, a dentist can identify early signs of occlusal trauma or manage gum inflammation, thereby creating better conditions for the body’s own maintenance systems to function optimally. Think of it as creating the best possible workshop for your body’s tiny repair crews to do their job when needed.
So, while the intricate work of cementum largely goes unnoticed, it’s a constant, quiet guardian of our tooth roots, diligently working to maintain their integrity against the minor challenges of daily life. Appreciating this hidden strength can motivate us to provide the supportive care our teeth deserve.