Often, when we think of teeth, the first thing that comes to mind is the hard, white enamel – the protective outer shell we see every day. But beneath this resilient surface lies a complex, living tissue that forms the bulk of the tooth: dentin. This remarkable layer is far more than just filler; it’s a dynamic, sensitive, and crucial component of dental structure and health. Understanding dentin provides a deeper appreciation for the intricate engineering of our teeth.
Unveiling Dentin: The Tooth’s Core Support
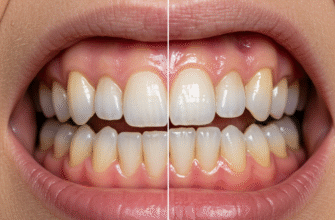
Dentin is located directly beneath the enamel in the crown of the tooth and under the cementum in the root. It essentially gives the tooth its shape and rigidity. If enamel is the armor, dentin is the supportive framework. It’s less mineralized and therefore less brittle than enamel, providing a degree of flexibility that helps prevent fractures under the forces of chewing. Its yellowish hue also contributes significantly to the overall color of a tooth, as enamel is relatively translucent. The thickness of the dentin layer varies, being thickest at the cusps or incisal edges and gradually thinning towards the root.
What’s Dentin Made Of? A Look at its Composition
Dentin is a calcified connective tissue, but its composition differs significantly from enamel and even bone. By weight, it’s approximately 70% inorganic material, primarily in the form of hydroxyapatite crystals, which are smaller than those found in enamel. About 20% is organic material, mainly Type I collagen, which forms a scaffold for the mineral crystals. The remaining 10% is water. This composition makes dentin harder than bone and cementum but softer and less wear-resistant than enamel. The organic component, particularly the collagen, gives dentin its resilience and toughness, a property enamel largely lacks.
Dentin is a vital, living tissue, characterized by microscopic channels called dentinal tubules. These tubules extend from the pulp cavity towards the outer enamel or cementum. They are fundamental to dentin’s unique properties, including its permeability and its role in tooth sensation, making it a dynamic interface within the tooth.
The Intricate Architecture: Tubules and Layers
The most striking feature of dentin is its microscopic structure, dominated by countless tiny channels known as dentinal tubules. These tubules radiate outwards from the pulp cavity (the tooth’s innermost chamber containing nerves and blood vessels) towards the enamel-dentin junction (DEJ) or the dentin-cementum junction (DCJ).
The Dentinal Tubules: Microscopic Highways
Dentinal tubules are not empty conduits. Each tubule typically contains an odontoblast process, which is a long, slender extension of an odontoblast cell. Odontoblasts are the specialized cells responsible for forming dentin, and their cell bodies line the periphery of the pulp cavity. The tubules also contain dentinal fluid, an extracellular fluid that is continuous with the fluid in the pulp. The density of these tubules is remarkable, estimated to be tens of thousands per square millimeter, being more densely packed and wider near the pulp and narrower and less dense towards the enamel or cementum. This structural arrangement is key to many of dentin’s characteristics, including its permeability and sensitivity.
There are distinct regions within the dentin based on proximity to these tubules.
Peritubular dentin (also known as intratubular dentin) is a highly calcified layer of dentin that lines the wall of each tubule. It is much more mineralized than the bulk of the dentin.
Intertubular dentin is the dentin located between the tubules, forming the main body of the tissue. It is less mineralized than peritubular dentin but still rich in collagen fibers.
Dentin formation, or dentinogenesis, is a process that continues, albeit at different rates, throughout a person’s life. This leads to the classification of dentin into several types based on when and how it is formed:
- Primary Dentin: This is the dentin formed before the completion of root development and tooth eruption. It constitutes the bulk of the tooth.
- Mantle Dentin: The outermost layer of primary dentin, found just beneath the enamel or cementum. It’s the first dentin formed by newly differentiated odontoblasts and is slightly less mineralized than the rest of primary dentin. Its collagen fibers are oriented perpendicular to the DEJ.
- Circumpulpal Dentin: This forms the majority of the primary dentin and is located around the pulp cavity, beneath the mantle dentin. Its collagen fibers are typically smaller and more randomly oriented than those in mantle dentin.
- Secondary Dentin: After the tooth erupts and the root is fully formed, dentin continues to be deposited slowly throughout life by the odontoblasts. This is secondary dentin. It is laid down on the pulpal side of the primary dentin, gradually reducing the size of the pulp chamber and root canals over time. Its structure is generally similar to primary dentin, but the tubules may show a slight change in direction. This is a normal physiological process.
- Tertiary Dentin (Reparative or Reactionary Dentin): This type of dentin forms in response to specific stimuli or irritants, such as wear, cavities, or dental procedures. It’s a protective mechanism by the pulp-dentin complex.
- Reactionary dentin is formed by pre-existing odontoblasts that survive the injury and upregulate their activity.
- Reparative dentin is formed by newly differentiated odontoblast-like cells when the original odontoblasts are damaged or die due to a more severe stimulus. Tertiary dentin is often less organized structurally than primary or secondary dentin, sometimes having fewer or more irregular tubules.
Properties That Define Dentin
Beyond its composition and structure, dentin exhibits several key properties:
Color: Dentin is naturally yellowish-white. Because enamel is semi-translucent, the color of the underlying dentin significantly influences the overall shade of the tooth. Thicker or darker dentin can make teeth appear more yellow.
Hardness and Elasticity: Dentin is considerably softer than enamel, making it more susceptible to wear if exposed. However, its lower mineral content and higher organic (collagen) content give it more elasticity and resilience. This elasticity is crucial as it provides a cushion for the brittle enamel, absorbing some of the shock from biting and chewing forces, thereby reducing the risk of enamel fracture.
Permeability: Due to the presence of dentinal tubules, dentin is a permeable tissue. These tubules can act as pathways for fluids, bacteria, and other substances to move from the oral environment towards the pulp, or vice versa. The permeability is generally higher closer to the pulp where tubules are wider and more numerous.
The Root of Sensitivity: Why Dentin Feels
One of the most well-known characteristics of dentin is its potential for sensitivity. When enamel wears away or gums recede, the underlying dentin can become exposed to the oral environment. This exposure is often the cause of tooth sensitivity to various stimuli.
The most widely accepted explanation for dentin sensitivity is the
hydrodynamic theory. This theory proposes that when exposed dentin is subjected to stimuli like temperature changes (hot or cold), osmotic changes (sugary or acidic foods), or tactile pressure (touching or brushing), it causes movement of the fluid within the dentinal tubules. This fluid movement is thought to stimulate nerve endings located in the pulp near the odontoblast layer, or possibly within the tubules themselves, leading to the sensation of pain or discomfort. The wider and more numerous the exposed tubules, the greater the potential for sensitivity.
Common triggers for dentin hypersensitivity include cold air or liquids, hot foods or drinks, sweet or sour substances, and even the pressure from a toothbrush bristle. It’s a sharp, sudden pain that is usually short-lived once the stimulus is removed.
The Dentin-Pulp Alliance: A Vital Connection
Dentin and pulp are not separate entities but rather form an integrated complex, often referred to as the
dentin-pulp complex. Their development and function are intimately linked. The odontoblasts, which produce dentin, have their cell bodies residing in the outermost layer of the pulp, while their processes extend into the dentinal tubules. This close physical and functional relationship means that whatever affects the dentin can potentially affect the pulp, and vice versa. For instance, if decay progresses through the enamel and reaches the dentin, the pulp can become inflamed due to the influx of bacteria and their byproducts through the permeable tubules.
Dentinogenesis: The Ongoing Creation
As mentioned, dentin formation (dentinogenesis) is carried out by specialized cells called odontoblasts. These cells differentiate from ectomesenchymal cells of the dental papilla during tooth development. They begin secreting an organic matrix called predentin, which is rich in collagen. This predentin subsequently mineralizes to become mature dentin. The odontoblasts retreat pulpally as they lay down dentin, leaving behind their cytoplasmic extensions within the forming tubules. This process is highly regulated and continues at a slow pace throughout life (as secondary dentin), and can be reactivated to form tertiary dentin in response to injury, highlighting the dynamic nature of this tissue.
Appreciating the Unseen Layer
Dentin is a truly remarkable tissue, playing a multifaceted role in the life of a tooth. It provides the bulk and shape, offers resilient support to the overlying enamel, houses the intricate network of tubules that contribute to its vitality and sensitivity, and maintains a close, lifelong relationship with the dental pulp. While often unseen, its health and integrity are paramount for overall tooth well-being. Understanding this sensitive layer beneath the enamel gives us a greater appreciation for the complexity and sophistication of our natural dentition.