The space often overlooked, yet constantly in use, is the
oral vestibule. Think of it as the antechamber to your main oral cavity, the area nestled between your lips and cheeks on the outside, and your teeth and gums on the inside. It’s this very region that first greets food and drink, and plays a crucial role in how we speak and express ourselves. While seemingly simple, this narrow C-shaped compartment is a dynamic zone, lined with a specialized membrane and housing several important small structures. It is the gateway, the initial point of contact for anything entering the mouth, setting the stage for further digestive processes or verbal communication.
Defining the Boundaries of the Vestibule
To truly understand the oral vestibule, we must first map out its borders. It’s a space defined by soft, mobile tissues externally and harder, more fixed structures internally. Visualizing these boundaries helps appreciate its form and function.
External Limits: Lips and Cheeks
The most obvious external boundaries are the
lips (labia) anteriorly and the
cheeks (buccae) laterally. The inner surfaces of your lips and cheeks directly form the outer wall of the vestibule. These structures are impressively muscular, primarily composed of the orbicularis oris muscle in the lips and the buccinator muscle in the cheeks. This muscular composition allows for the incredible range of motion needed for eating, sucking, whistling, speaking, and forming facial expressions. The transition from the outer, keratinized skin of the lips to the moist inner lining (mucosa) occurs at the vermilion border, a distinct landmark that is unique to humans. Inside the mouth, this mucosal lining continues, forming the pliable, distensible outer wall of the vestibule. The flexibility of these tissues means the volume of the vestibule can change dramatically.
Internal Limits: Teeth and Gums
Moving inwards, the vestibule is bounded by the
teeth and the
gingiva (gums) that surround them. When your mouth is closed and teeth are in normal occlusion (biting together), the vestibule is a relatively small, slit-like potential space. However, it can expand considerably, for example, when you puff out your cheeks or when a dentist needs to access the area. The gingiva, the firm, stippled, pink tissue that covers the alveolar bone supporting the teeth, forms a critical part of this inner boundary. This tissue is specialized to withstand the forces of chewing and protect the underlying bone and tooth roots.
Superior and Inferior Extents: The Mucobuccal and Mucolabial Folds
The top (superior) and bottom (inferior) limits of the vestibule are formed by a reflection, or a turning point, of the mucosal lining. This lining extends from the inner surface of the lips and cheeks and then folds back onto itself to cover the alveolar bone and become the gingiva. These U-shaped troughs are known as the
mucobuccal fold (laterally, alongside the cheeks) and the
mucolabial fold (anteriorly, behind the lips). The deepest part of this trough is often called the fornix of the vestibule. The depth of these folds can vary significantly between individuals and even in different parts of the same person’s mouth. For instance, it might be deeper in the molar region compared to the incisor region.
The oral vestibule is essentially a C-shaped space when viewed from the front with the mouth slightly open, with the opening between the lips forming the entrance. It communicates with the oral cavity proper (the space inside the arches of the teeth) primarily through the spaces between the teeth (interdental spaces) and, when the mouth is open, more broadly behind the last molars in an area called the retromolar space. This anatomical arrangement is key to its function in food manipulation and hygiene.
The Lining: A Specialized Mucous Membrane
The entire oral vestibule is lined by a
mucous membrane, often referred to simply as oral mucosa. This isn’t just any lining; it’s a specialized, resilient tissue perfectly adapted to the unique and challenging environment of the mouth. It’s typically moist, relatively soft, and plays both protective and sensory roles, constantly interfacing with food, liquids, and air.
Epithelial Layer
The outermost layer of this mucosa is
stratified squamous epithelium. ‘Stratified’ means it’s composed of multiple layers of cells, stacked one upon another, offering robust protection against the friction from food particles during chewing and other mechanical stresses, such as those from tooth brushing. ‘Squamous’ refers to the flattened, scale-like shape of the cells in the uppermost layers. For the most part, the epithelium lining the vestibule is
non-keratinized. This means it lacks the tough, fibrous, waterproof protein called keratin that is found in the epidermis of the skin and in certain parts of the oral mucosa that experience more direct and intense abrasion, like the hard palate and the attached gingiva. The non-keratinized nature contributes to its softer, more pliable texture and its characteristic reddish-pink hue, as the underlying blood vessels are more visible through the thinner, less opaque epithelial layers.
Connective Tissue and Blood Supply
Beneath the epithelium lies a layer of connective tissue called the
lamina propria. This layer is rich in collagen and elastic fibers, providing support and flexibility to the mucosa. It is also highly vascularized, containing an extensive network of blood vessels which supply oxygen and nutrients to the avascular epithelium and contribute significantly to the mucosa’s pink or red color. Furthermore, the lamina propria contains numerous nerve fibers, making the vestibular lining sensitive to touch, temperature, pain, and taste (though taste buds are generally not prominent in the vestibule itself, but on the tongue). Small elastic fibers within the lamina propria allow the mucosa to stretch and recoil as the lips and cheeks move dynamically during speech and mastication. Deeper still, a
submucosa is generally present in the vestibular regions lining the lips and cheeks. This layer contains larger blood vessels, nerves, adipose (fat) tissue which provides cushioning, and the bodies of minor salivary glands.
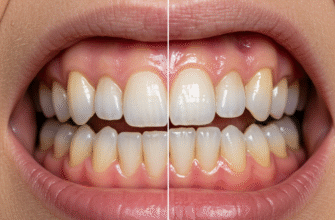
Color and Texture
The healthy vestibular mucosa is typically pinkish-red, though its exact shade can vary with an individual’s complexion, degree of pigmentation (melanin content), and the density of the underlying vascular bed. It should appear smooth and glisteningly moist. The presence of numerous minor salivary glands, embedded within the submucosa of the lips (labial glands) and cheeks (buccal glands), constantly secretes small amounts of saliva (primarily mucous saliva) directly onto its surface. This continuous lubrication is vital for keeping it supple, protecting it from desiccation, and aiding in its protective functions against minor irritants and microbes.
The mucous membrane of the oral vestibule is relatively delicate compared to the skin or even the keratinized portions of the oral cavity. It is well-vascularized, which means it can bleed somewhat easily if traumatized by sharp foods or accidental bites. Maintaining good oral hygiene practices is important to keep this lining healthy, free from inflammation, and capable of performing its protective duties effectively.
Key Structures Housed Within the Vestibule
Despite its seemingly simple nature as a “space,” the oral vestibule contains several specific anatomical structures that are vital for its function and for overall oral health. These are not just passive occupants but active contributors to the oral environment, each with a defined role.
Frenula: The Guiding Tethers
Prominent among these structures are the
frenula (singular: frenulum or frenum). These are distinct, often V-shaped folds of mucous membrane, containing some fibrous connective tissue and occasionally muscle fibers, that extend from the inner alveolar mucosa lining the jawbone to the inner surface of the lips and cheeks. They act like tethers or guy ropes, restricting excessive movement of the lips and cheeks and providing stability to these mobile structures relative to the fixed jaws.
- Superior Labial Frenulum: This is usually the most prominent frenulum. It’s a midline fold connecting the inner surface of the upper lip to the alveolar mucosa and gingiva between the upper central incisor teeth. Its size, thickness, and the exact point of its gingival attachment can vary considerably among individuals. A very prominent or low-attaching superior labial frenulum can sometimes be associated with a gap (diastema) between the front teeth, and in some cases, may warrant clinical attention if it causes issues.
- Inferior Labial Frenulum: Similar to its superior counterpart, this midline fold connects the inner surface of the lower lip to the alveolar mucosa and gingiva between the lower central incisors. It is generally less prominent and thinner than the superior labial frenulum.
- Buccal Frenula: There are also typically smaller, less defined frenula located laterally in the vestibule, connecting the inner cheek mucosa to the gingiva in the canine or premolar regions of both the upper and lower jaws. These help to anchor the cheek mucosa and limit its excursion during function. There can be one or more on each side, in each jaw.
The tension and attachment of these frenula are important. If they are too tight, too broad, or attached too close to the edge of the gums (the gingival margin), they can sometimes exert a pull on the gingival margin during lip or cheek movement. This pulling action might, in susceptible individuals with thin gum tissue, contribute to localized gum recession or interfere with proper toothbrushing in the area, although this is a complex issue with multiple contributing factors.
Openings of Salivary Glands: Nature’s Lubricators
The vestibule is a key site for the entry of saliva into the mouth, which is essential for lubrication, initiating digestion, taste, speech, and protection of oral tissues.
- Parotid Duct Opening (Stensen’s Duct): One of the most significant structures is the opening of the parotid duct. The parotid gland, the largest of the three pairs of major salivary glands, is located primarily in the retromandibular fossa, in front of and below the ear. Its duct, known as Stensen’s duct, is about 5-7 cm long and travels forward across the outer surface of the masseter muscle, then turns sharply inwards to pierce the buccinator muscle of the cheek. It finally opens into the oral vestibule. This opening is typically found on a small, distinct elevation of mucosa called the parotid papilla. This papilla is strategically located on the inner surface of the cheek, opposite the crown of the maxillary (upper) second molar tooth. You might even be able to feel this small bump with your tongue or see it if you retract your cheek.
- Minor Salivary Glands: Besides the major glands, the mucosa lining the lips (labial glands) and cheeks (buccal glands) is peppered with hundreds of minor salivary glands. These small, independent exocrine glands are embedded within the submucosa and have tiny, individual ducts that open directly onto the surface of the vestibular mucosa. While each one contributes only a minuscule amount of saliva (mostly mucous in nature, which is thick and lubricating, but some can be serous or mixed), their collective output is significant. They are responsible for keeping the vestibular surfaces constantly moist and lubricated, which is crucial for comfortable speech, easy movement of lips and cheeks over teeth, and for protecting the tissues from drying out or minor frictional trauma.
Alveolar Mucosa and Gingiva
While the gingiva forms the inner boundary of the vestibule, the transition zone from the looser, redder, more mobile
alveolar mucosa (which covers the alveolar bone further from the teeth) to the firmer, pinker, stippled
attached gingiva (which is tightly bound to the teeth and underlying periosteum of the alveolar bone) often occurs within the visual field of the vestibule. This demarcation, known as the
mucogingival junction, is an important anatomical landmark. The alveolar mucosa is thin and allows the color of underlying blood vessels to show through, giving it a redder appearance compared to the paler pink of the attached gingiva.
Functional Significance: More Than Just Space
The oral vestibule is far more than a passive conduit; it actively participates in several critical oral functions. Its unique anatomy, with mobile outer walls (lips and cheeks) and a relatively fixed inner boundary (teeth and gums), facilitates these diverse and essential roles.
Initial Food Processing and Mastication
When food enters the mouth, the vestibule is the first intraoral space it occupies. The lips and cheeks, forming the outer wall of the vestibule, are crucial for several aspects of eating:
- Food Intake and Containment: The lips (orbicularis oris muscle) create a seal to take in food and liquid and prevent it from dribbling out of the mouth.
- Food Manipulation: During chewing (mastication), the muscles of the cheeks (especially the buccinator) and lips work in precise coordination with the tongue. Their primary role here is to keep the bolus of food on the occlusal (chewing) surfaces of the teeth. They constantly push food that strays into the vestibule back towards the dental arches. Without this efficient action, food would accumulate in the vestibule, making efficient chewing difficult and prolonged.
- Temporary Reservoir: The vestibule can act as a temporary holding space or “pouch” for food before it is fully processed by the teeth or moved further back into the oral cavity proper for swallowing. This is particularly evident with the cheek pouches of some animals, but humans also utilize this space to a lesser extent.
Speech and Articulation
The lips are primary articulators for producing many consonant and vowel speech sounds (e.g., bilabial sounds like ‘p’, ‘b’, ‘m’; labiodental sounds like ‘f’, ‘v’; and lip-rounded vowels like ‘oo’, ‘oh’). The precise shape and movement of the lips, controlled by complex facial musculature, modify the airflow from the lungs and larynx to create these distinct phonetic units. The vestibule is the immediate space behind the lips that is shaped and altered during these articulatory movements. The ability of the cheeks to maintain tone and prevent excessive bulging also subtly influences the resonance and clarity of speech.
Saliva Distribution and Oral Hygiene
As previously mentioned, the parotid duct and numerous minor salivary glands open directly into the vestibule. This strategic placement ensures that saliva, particularly the serous saliva from the parotid gland which is rich in enzymes like amylase, and the mucous saliva from minor glands, is efficiently distributed over the buccal and labial surfaces of the teeth and the mucosal surfaces themselves. Saliva performs many functions:
- It lubricates these tissues, facilitating smooth movement and speech.
- It aids in the initial stages of digestion by beginning carbohydrate breakdown.
- It helps in taste perception by dissolving food substances so they can interact with taste buds.
- It possesses antimicrobial properties (e.g., lysozyme, lactoferrin, IgA) and acts as a buffer, contributing to oral hygiene by washing away food debris, neutralizing acids produced by plaque bacteria, and aiding in the remineralization of tooth enamel.
Sensory Perception
The rich sensory nerve supply to the vestibular mucosa, derived from branches of the trigeminal nerve, makes it highly sensitive to touch, pressure, temperature, and pain. This sensory feedback is important for:
- Detecting the consistency, texture, and temperature of food items, helping to prepare for mastication.
- Providing protective reflexes, such as withdrawing from excessively hot or sharp objects, preventing injury.
- Contributing to the overall sensory experience of eating and drinking, which influences food enjoyment and satiety.
The coordinated action of the lips, cheeks, and tongue, with the vestibule as the operational arena, is absolutely essential for efficient mastication and deglutition (swallowing). This complex neuromuscular activity prevents food from simply falling out of the mouth or getting lost in the “corners” of the vestibule. The constant moisture provided by salivary glands opening here is also paramount for tissue comfort, health, and optimal function.
A Few General Considerations
The oral vestibule, while generally consistent in its basic anatomical plan across humans, can exhibit variations among individuals. The
depth of the vestibule, for instance, meaning the vertical distance from the crest of the alveolar ridge (or the gingival margin if teeth are present) to the height of the mucobuccal or mucolabial fold, can differ quite a bit. This dimension can be influenced by factors such as the amount and shape of underlying alveolar bone, the thickness of the overlying soft tissues, the height of muscle attachments (like the mentalis muscle in the lower lip region), and even an individual’s age and dental status.
Over time, with natural aging processes or due to changes in dental status (like tooth loss and subsequent bone resorption), the anatomy of the vestibule can also undergo modifications. For example, significant resorption of the alveolar bone after teeth are lost can lead to a shallower vestibule and a change in the relationship of the mobile tissues to the underlying bone. The elasticity and tone of the tissues of the lips and cheeks may also change with age, affecting the pliability and overall contour of the vestibule.
Understanding the general layout of the oral vestibule is fundamental not just for academic interest but also forms a basis for various dental and medical observations and procedures. Its accessibility makes it an area that is readily examined visually and by palpation. The health of its lining often reflects overall systemic health and oral hygiene practices. For instance, certain vitamin deficiencies or systemic conditions can manifest with changes in the oral mucosa, including that of the vestibule. The presence and normalcy of the parotid papilla is a key landmark, and the integrity and attachment levels of the frenula are also noted during routine oral examinations. This area is also a common site for the administration of local anesthetics in dentistry.
The vestibule is a dynamic and sensitive area, constantly adapting to use and reflecting bodily states. Its dimensions and the feel of its tissues can provide clues during a clinical examination, but this article serves only as a general anatomical overview and not as a diagnostic guide. Any specific concerns about your oral health, or any unusual changes noted in the oral vestibule, should always be directed to a qualified healthcare professional, such as a dentist or doctor, for proper evaluation and guidance.
In essence, the oral vestibule is a small but mighty compartment within the complex architecture of the head and neck. It’s the gateway to the digestive system, a crucial player in communication, and a meticulously designed space that showcases the intricate functionality and adaptability of human anatomy. Its surfaces are constantly bathed in saliva, touched by food and drink, shaped by our expressions, and serve as the first line of interaction with the external environment through the mouth, making it a truly active and essential part of our daily lives and well-being.